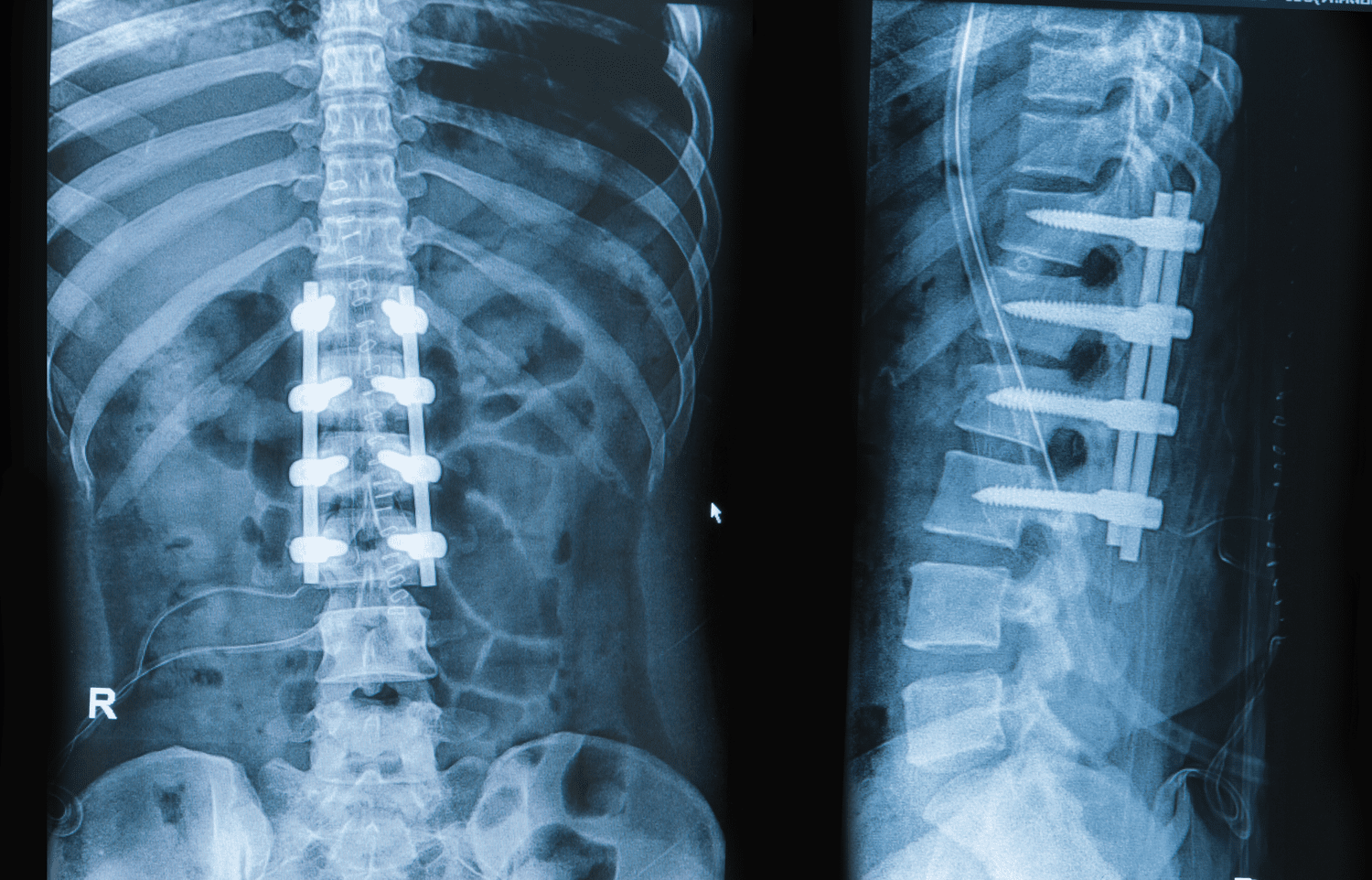
A spinal fusion, often a last resort for chronic and debilitating back pain or spinal instability, represents a profound intervention. It’s a surgical procedure designed to permanently connect two or more vertebrae in the spine, eliminating motion between them. While the goal is to stabilize the spine and alleviate pain, the journey of rebuilding life after a spinal fusion is far from instantaneous. It’s a marathon, not a sprint, demanding patience, perseverance, and a meticulous adherence to rehabilitation protocols. Many individuals envision immediate relief and a quick return to their previous activities, only to discover that the recovery process is multifaceted, encompassing physical, emotional, and psychological adjustments. The success of the surgery itself is just one piece of the puzzle; the true measure of recovery lies in how effectively one navigates the post-operative landscape, adapting to a new normal and gradually reclaiming a fulfilling life. Understanding this intricate recovery process is crucial, as it sets realistic expectations and empowers patients to actively participate in their own healing, moving beyond simply mending bones to truly mending lives.
The Immediate Aftermath: Navigating Post-Operative Pain and Care
The initial phase of recovery begins with the immediate aftermath, centered on navigating post-operative pain and care. Waking up from spinal fusion surgery often involves a significant level of pain, managed through a carefully tailored regimen of intravenous and oral pain medications. The goal is not to eliminate pain entirely but to make it tolerable enough for early mobilization. Patients will typically spend a few days in the hospital, where nurses and physical therapists provide essential guidance on safe movement, emphasizing proper body mechanics for getting in and out of bed, walking, and using the bathroom. Incision care is critical to prevent infection, and patients are taught how to keep the surgical site clean and dry. There might be some initial numbness or tingling, which usually subsides. Understanding that this acute phase is about stabilization and initial healing, rather than expecting complete pain freedom, is key. This careful navigating of post-operative pain and care sets the stage for the longer recovery journey, ensuring foundational healing and pain management are prioritized.
Early Mobilization: The Crucial First Steps to Recovery
Despite the pain and initial stiffness, early mobilization represents the crucial first steps to recovery. While rest is important, prolonged bed rest is generally discouraged after spinal fusion due to the risk of complications like blood clots, pneumonia, and muscle deconditioning. Under the guidance of physical therapists, patients are encouraged to get out of bed and walk short distances within a day or two of surgery. These initial walks are slow and tentative but incredibly important. They help improve circulation, reduce swelling, and prevent stiffness. The therapists will teach specific techniques for moving the spine as a unit, avoiding twisting or bending, which are strictly prohibited. These gentle movements are not about pushing limits but about reactivating muscles and promoting blood flow to the surgical site, aiding the healing process. This phase is about learning how to move safely within new restrictions, emphasizing that the crucial first steps to recovery lie in carefully controlled early mobilization.
Understanding Spinal Fusion: The Biology of Bone Growth
A key aspect of recovery is understanding spinal fusion, particularly the biology of bone growth. Spinal fusion isn’t merely about bolting bones together; it’s about creating an environment where two or more vertebrae can biologically fuse into a single, solid bone segment. This process, called arthrodesis, relies on bone grafts, which can be autograft (taken from the patient’s own body), allograft (from a donor), or synthetic materials. The bone graft acts as a bridge, stimulating new bone cells to grow across the space between the vertebrae. This takes time, often several months, for the new bone to form and consolidate. During this period, the fusion site is vulnerable, and patients must strictly adhere to restrictions on bending, lifting, and twisting. The success of the fusion is paramount, as a “non-union” (where the bones don’t fuse) can lead to continued pain and potentially require further surgery. Grasping the biology of bone growth helps patients appreciate why patience and strict adherence to post-operative instructions are vital for a successful spinal fusion.
Physical Therapy’s Pivotal Role: Rebuilding Strength and Function
Beyond immediate post-op care, physical therapy’s pivotal role becomes central to rebuilding strength and function. Once the initial healing phase is underway, typically a few weeks after surgery, a more structured physical therapy program begins. This program is highly individualized, progressing gradually. It focuses on strengthening the core muscles (abdominals, back muscles, glutes) that provide stability to the spine, as well as improving overall flexibility in adjacent spinal segments and other joints. Therapists guide patients through exercises designed to improve balance, coordination, and endurance. They also educate on proper posture, lifting techniques, and body mechanics to protect the fused segment and prevent injury to other parts of the spine. The goal is not just to reduce pain but to restore functional independence, enabling patients to return to daily activities, work, and even recreational pursuits safely. This dedicated effort in rebuilding strength and function makes physical therapy’s pivotal role indispensable for a robust recovery.
Managing Expectations: A Realistic Outlook for Recovery Time
One of the most challenging aspects of this journey is managing expectations, cultivating a realistic outlook for recovery time. Spinal fusion recovery is not a sprint; it’s a marathon that often spans many months, sometimes even a year or more, before full benefits are realized. Initial pain relief is gradual, and some discomfort is normal for an extended period. Patients need to understand that while movement is encouraged, strenuous activities, heavy lifting, and impact sports are typically restricted for several months to allow the fusion to solidify. Fatigue is also a common and often underestimated part of the recovery, as the body expends significant energy on healing. Setting small, achievable goals and celebrating incremental progress, rather than expecting a rapid return to pre-surgery activity levels, is crucial for maintaining morale. This commitment to a realistic outlook for recovery time is vital for successful long-term outcomes and prevents frustration arising from unrealistic managing expectations.
Addressing Psychological Impact: Battling Frustration and Fear
Beyond the physical, addressing psychological impact is critical for battling frustration and fear. Chronic pain, the stress of surgery, and the lengthy recovery period can take a significant toll on mental well-being. Patients might experience feelings of frustration over limitations, fear of re-injury, anxiety about the future, or even depression. It’s common to mourn the loss of certain abilities or activities. Open communication with family, friends, and healthcare providers is vital. Some individuals may benefit from counseling, support groups, or mindfulness techniques to cope with the emotional challenges. Setting realistic goals, focusing on small victories, and maintaining a positive attitude are important. Recognizing and proactively battling frustration and fear through mental health support is as crucial as physical rehabilitation, ensuring that the patient’s emotional well-being is cared for during the recovery process.
Lifestyle Adjustments: Adapting to a New Spinal Reality
Life after spinal fusion often requires lifestyle adjustments, a process of adapting to a new spinal reality. While the goal is to restore function, the fused segment of the spine will no longer move. This means that adjacent spinal segments may experience increased stress over time. Patients are often advised to continue practicing good body mechanics, maintaining a healthy weight, and staying physically active with appropriate exercises to protect the rest of their spine. Activities involving repetitive bending, lifting heavy objects, or high-impact movements might need to be modified or avoided long-term. Ergonomic adjustments at work and home are often recommended. For some, this might mean finding new ways to enjoy hobbies or sports. It’s not about permanent disability, but about understanding and adapting to a new spinal reality through proactive lifestyle adjustments that support the longevity of the fusion and overall spinal health.
Nutrition and Healing: Fueling the Fusion Process
A frequently underestimated factor in recovery is nutrition and healing, specifically fueling the fusion process. Adequate nutrition provides the essential building blocks for bone growth and tissue repair. A diet rich in protein, calcium, Vitamin D, and other vital minerals supports the fusion process. Lean meats, fish, dairy products, leafy greens, and fortified foods are important. Avoiding smoking is absolutely critical, as nicotine severely impairs bone healing and significantly increases the risk of non-union. Similarly, excessive alcohol consumption can hinder recovery. Maintaining good hydration is also important for overall bodily function and tissue health. A well-balanced diet not only supports the physical healing of the surgical site but also contributes to overall energy levels and well-being, providing the necessary elements for fueling the fusion process and optimizing nutrition and healing.
Return to Activities: A Phased and Monitored Process
The journey back to normalcy involves return to activities, a phased and monitored process. This is never a sudden leap but a gradual reintroduction of movements and responsibilities. Light daily activities typically resume within weeks, but strenuous activities, including heavy lifting, vigorous exercise, and contact sports, are usually restricted for several months, often until the fusion is radiographically confirmed to be solid. Physical therapists play a crucial role in guiding this progression, ensuring that activities are introduced safely and progressively, minimizing the risk of re-injury or strain on the recovering spine. Patients are taught how to listen to their bodies and avoid pain-inducing movements. This disciplined, phased and monitored process is essential for a successful and sustainable return to activities, allowing the patient to gradually and safely reclaim their desired level of function and lifestyle.
Long-Term Management: Sustaining Spinal Health
Even after recovery, long-term management is key to sustaining spinal health. Spinal fusion, while effective for specific conditions, changes the biomechanics of the spine. Adjacent segment disease, where increased stress on the vertebrae above and below the fusion leads to degeneration, is a potential long-term concern. Regular follow-up appointments with the spine surgeon are important to monitor the fusion site and overall spinal health. Continuing a modified exercise program, maintaining a healthy weight, and practicing good posture remain lifelong commitments. Being mindful of body mechanics during daily tasks and seeking early intervention for any new back pain are also crucial. This proactive sustaining spinal health through vigilant long-term management allows individuals to optimize the benefits of their spinal fusion and minimize future spinal issues, preserving their mobility and quality of life for years to come.